Cluster headache, migraine strongly associated with circadian system, according to published research
March 29, 2023 By: Caitie Barkley
Cluster headache and migraine are both strongly linked to the internal clock that regulates body processes known as the circadian system, according to new research from UTHealth Houston.
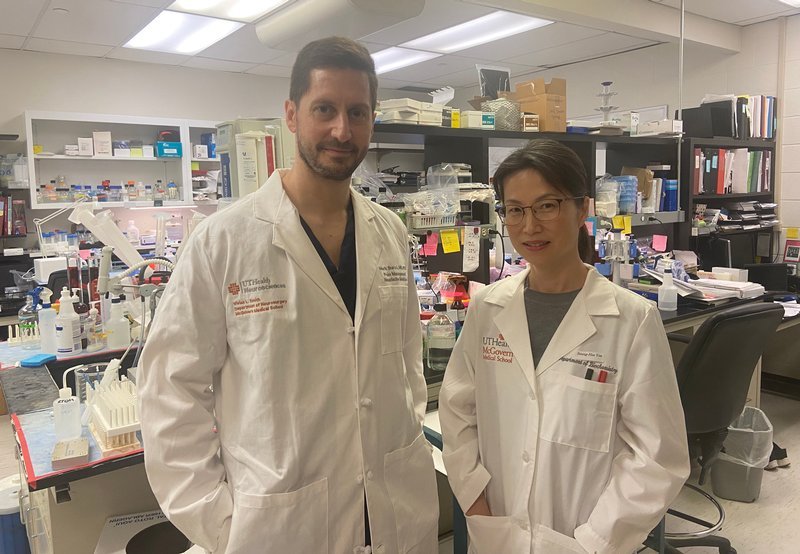
A study led by Mark J. Burish, MD, PhD, associate professor in the Vivian L. Smith Department of Neurosurgery with McGovern Medical School at UTHealth Houston, and Seung-Hee Yoo, PhD, associate professor in the Department of Biochemistry and Molecular Biology with the medical school, analyzed all available research on cluster headache and migraine that included circadian features, such as information on the timing of headaches during the day and during the year, whether genes associated with the circadian clock are more common in people with these headaches, and hormones linked to both the circadian system and the headaches.
Their findings were published online on March 29, 2023 in Neurology, the medical journal of the American Academy of Neurology.
“We became interested in this topic because some of our patients here at UTHealth Houston, and many cases in the literature, report headaches that happen at the same time each day,” said Burish, who is also a faculty member with The University of Texas MD Anderson Cancer Center UTHealth Houston Graduate School of Biomedical Sciences. “We wanted to investigate that more, and we were surprised at just how much these headaches are linked to the circadian clock.”
A circadian pattern of cluster headache attacks was found in more than 70% of participants across 16 studies, with a clear circadian peak between 9 p.m. and 3 a.m. and seasonal peaks in spring and autumn. The pattern is highly precise, varying by only minutes day-to-day in many patients.
People with cluster headache were also found to have lower levels of melatonin and higher levels of cortisol in their system. At the cellular level, cluster headache was associated with core circadian genes CLOCK and REV-ERBα, and five of the nine genes tied to cluster headache susceptibility were clock-controlled genes.
For migraines, the analysis showed a circadian pattern of attacks in 50% of participants across eight studies, with a clear circadian trough, or lowest point of activity, between 11 p.m. and 7 a.m. and a broad seasonal peak between April and October.
Migraine participants had lower urinary melatonin levels, which dropped even lower during an attack. Migraine was also associated with core circadian genes CK1δ and RORα, and 110 of the 168 migraine susceptibility genes were clock-controlled.
By offering further insight into the circadian features of both headache disorders, Burish said his findings provide a pathophysiological foundation for circadian-targeted research into cluster headache and migraine.
“A better understanding of headache timing might eventually lead to medications that prevent the headaches at those times or manage painful episodes better,” Yoo said.
While cluster headaches and migraines are similar, there are some key differences between them. Unlike migraines, which can last an entire day or potentially several days if left untreated, cluster headaches typically last anywhere from 15 to 180 minutes. Additionally, though it is uncommon to have more than one migraine a day, it is possible for someone to have up to eight cluster headaches over a 24-hour period. Migraine pain can vary by location; in contrast, cluster headaches involve only one side of the head, typically at the temple or around the eye. Lastly, people who have migraines tend to rest in a quiet, dark room, whereas people who have cluster headaches tend to become restless and often pace around the room.
The study received funding from the Will Erwin Headache Research Foundation.
Media Inquiries: 713-500-3030







